Nipah Virus Explained: Symptoms, Spread & India Alert
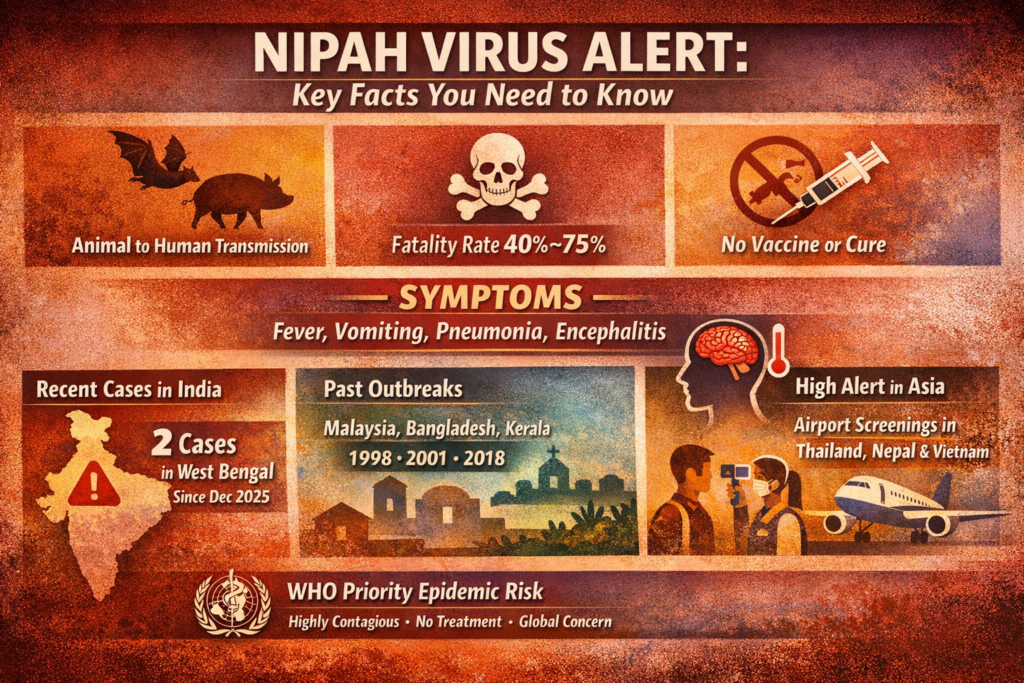
Nipah Virus Explained: What You Must Know as Asia Tightens Health Alerts Quick Summary (Key Facts at a Glance) Nipah virus is a highly deadly zoonotic disease that spreads from animals to humans Fatality rate ranges between 40%–75%, with no approved vaccine or treatment Two confirmed cases have been reported in West Bengal, India, since December Virus spreads via fruit bats, pigs, contaminated food, and human-to-human contact Symptoms range from fever and vomiting to pneumonia and brain inflammation Asian countries have increased airport and border screenings as a precaution WHO classifies Nipah as a top-priority epidemic threat What Is the Nipah Virus? The Nipah virus is a severe and often fatal infectious disease caused by a zoonotic virus. It primarily spreads from animals—especially fruit bats and pigs—to humans. In some cases, it can also transmit between people, making it a serious public health concern. The World Health Organization (WHO) lists Nipah among its top ten priority diseases due to its epidemic potential, high mortality rate, and lack of medical countermeasures. Why Is Nipah Virus So Dangerous? Nipah virus is considered exceptionally dangerous for three key reasons: High fatality rate: Between 40% and 75% of infected individuals die No vaccine or cure: Treatment is limited to supportive care only Human-to-human transmission: Outbreaks can escalate quickly if not contained Unlike many viral infections, Nipah can attack both the respiratory system and the brain, leading to rapid deterioration in severe cases. How Does Nipah Virus Spread? Transmission occurs through multiple pathways: Direct contact with infected animals such as fruit bats or pigs Consumption of contaminated food, including raw date palm sap Exposure to bodily fluids of infected individuals Close contact in healthcare or household settings Fruit bats are considered the natural reservoir of the virus, often contaminating food sources without visible signs of illness. Symptoms and Incubation Period The incubation period typically ranges from 4 to 14 days, though symptoms may vary in severity. Early symptoms include: High fever Headache and muscle pain Nausea and vomiting Sore throat and fatigue Severe complications may include: Pneumonia and breathing difficulties Altered consciousness and confusion Seizures Encephalitis (brain inflammation), which can be fatal Some infected individuals may initially show mild or no symptoms, complicating early detection. History of Nipah Virus Outbreaks 1998–1999 (Malaysia & Singapore): First outbreak among pig farmers; over 100 deaths 2001 onwards (Bangladesh): Recurrent outbreaks linked to raw date palm sap India: West Bengal outbreaks in 2001 and 2007 Kerala outbreaks in 2018 (17 deaths) and 2023 Bangladesh remains one of the most affected countries, with over 100 deaths reported since 2001. What Is Happening in India Now? India has confirmed two Nipah virus cases in West Bengal since December. Health authorities reported: Nearly 200 close contacts were traced and tested negative No evidence of wider community spread Enhanced surveillance and laboratory testing in affected areas The Indian health ministry has emphasized that reports of a surge are inaccurate and that the situation remains under control. Why Are Asian Airports on High Alert? Although no cases have been detected outside India, several countries have adopted precautionary measures: Thailand: Screening passengers at major airports, health declarations required Nepal: Enhanced checks at airports and land borders Vietnam & Indonesia: Temperature screenings for travelers from India Taiwan: Proposed classification of Nipah as a high-risk emerging disease Myanmar: Advisory against nonessential travel to West Bengal These steps aim to prevent cross-border transmission and ensure early detection. Current Global Risk Assessment Health officials stress that while the virus is deadly, early detection and containment are effective. So far, the limited number of cases and rapid response suggest the outbreak is contained. However, due to Nipah’s high mortality rate and epidemic potential, global health agencies continue to monitor the situation closely. Bottom Line Nipah virus is rare but extremely dangerous. With no vaccine and a high fatality rate, prevention, surveillance, and rapid response remain the strongest defenses. While current cases in India appear contained, heightened vigilance across Asia reflects the seriousness of the threat. References: https://www.theguardian.com/science/2026/jan/28/what-is-nipah-virus-outbreak-india-symptoms https://www.bbc.com/news/articles/cd7zp581q5do https://www.washingtonpost.com/world/2026/01/27/nipah-virus-outbreak-india/
Nipah Virus Explained: Symptoms, Spread & India Alert Read More »